Corneal Dystrophies and Scars
Corneal dystrophies are inherited conditions that affect the clarity of the cornea. Corneal scars are opacities that affect the clarity of the cornea and consequently, the vision.
Call Us: 215-928-3180
Corneal dystrophies are inherited conditions that affect the clarity of the cornea. Corneal scars are opacities that affect the clarity of the cornea and consequently, the vision.
Call Us: 215-928-3180
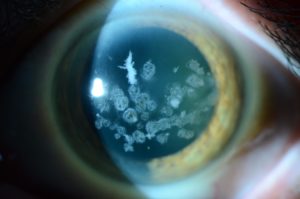 Corneal dystrophies are inherited conditions that affect the clarity of the cornea. They usually affect both eyes and can involve the front, middle, or back layers of the cornea. They tend to get worse over time.
Corneal dystrophies are inherited conditions that affect the clarity of the cornea. They usually affect both eyes and can involve the front, middle, or back layers of the cornea. They tend to get worse over time.

Corneal scars are opacities that affect the clarity of the cornea and consequently, the vision. Scars can result from corneal infection, trauma, or other reasons.
Depending on the severity, location, and depth of the opacity, these corneas can be treated with surgical removal with a blade or laser (phototherapeutic keratectomy or PTK) (see “Surgical Procedures” page), or partial or full thickness corneal transplantation (see “Surgical Procedures” page).
Corneal dystrophies are inherited conditions that affect the clarity of the cornea. Corneal scars are opacities that affect the clarity of the cornea and consequently, the vision.
The most common symptom is decreased vision. Some dystrophies such as Fuchs' dystrophy can cause fluctuating vision that tends to be worse in the mornings. Other dystrophies, such as Reis-Bucklers and lattice corneal dystrophies can cause painful episodes (corneal erosions). Corneal scarring can cause decreased vision from direct blockage of the vision from the opacity or warping of the image from corneal irregularity.
Corneal dystrophies are generally inherited conditions, but there may or may not be a family history of the disease, depending on the dystrophy and the family. Corneal scarring tends to come from an insult to the cornea, such as trauma or infection (corneal ulcer).
Family history of corneal dystrophy. Contact lens wear and eye trauma are the main risk factors for corneal infections.
Corneal erosions can predispose to corneal infection.
The diagnosis can usually be made during a slit lamp examination. Ancillary testing includes corneal curvature and thickness mapping (corneal topography and tomography) and measurement of the corneal thickness (pachymetry). Anterior segment optical coherence tomography (AS-OCT) may be helpful in some cases. Genetic testing may be considered in patients with inherited corneal dystrophies.
Mild cases may just require routine observation. More severe cases may require contact lenses to improve vision. Soft toric lenses, rigid gas permeable lenses, piggyback, hybrid (e.g. Synergeyes), or scleral (e.g. PROSE) lenses may be used. If the corneal dystrophy opacities or scarring is fairly superficial, a laser (excimer laser) may be able to remove some or all of the opacity with a procedure called phototherapeutic keratectomy (PTK) (see “Surgical Procedures” page). Corneal transplantation (either partial thickness or full thickness) can be very successful for patients who don’t do well with contact lenses.
Routine eye examinations are recommended to monitor the condition.
