Ocular Surface Disease
Damage to the epithelium can cause pain, redness, poor vision, and ultimately can lead to permanent corneal or conjunctival injury. Treatment depends on the underlying cause of the ocular surface disease.
Call Us: 215-928-3180
Damage to the epithelium can cause pain, redness, poor vision, and ultimately can lead to permanent corneal or conjunctival injury. Treatment depends on the underlying cause of the ocular surface disease.
Call Us: 215-928-3180
The surface layers of the eye consist of the conjunctiva (clear covering of the white of the eye) and the cornea (clear covering over the colored iris and black pupil). These are both covered with a layer called the epithelium. In eyes with ocular surface disease, this epithelial layer is damaged. This damage may result from a wide variety of conditions involving the eye, the eyelids, and even the rest of the body. Damage to the epithelium can cause pain, redness, poor vision, and ultimately can lead to permanent corneal or conjunctival injury. Treatment depends on the underlying cause of the ocular surface disease.
Dry eye syndrome is often a chronic condition primarily caused by poor quality or quantity of tears. It can usually be controlled with treatment. The most common symptoms of dry eye syndrome are a dry, gritty, sandy sensation in the eyes, but symptoms also include redness, mucous discharge, fluctuation of vision, contact lens intolerance, and ironically, excess tearing.
Many of these symptoms can also be caused by other ocular conditions such as blepharitis (inflammation of the eyelids) and ocular allergies. Dry eye symptoms are often made worse by activities where patients tend not to blink frequently, such as reading, working on the computer, and watching television. Dry eye symptoms are also generally worse toward the end of the day.
There is a stepwise approach treatment of dry eyes generally beginning with artificial teardrops, gels and ointments, cyclosporine drops (e.g. Restasis or Cequa), lifitegrast drops (e.g. Xiidra), and punctal plugs. Changing the local environment such as using humidifiers and staying away from drafts can also be very helpful. Other treatments include cautery of the tear drainage ducts (when plugs aren’t staying in), Lacriserts, acetylcysteine (Mucomyst) for mucous filaments, and permanent partial closure of the eyelids (small lateral tarsorrhaphy).
 haritis
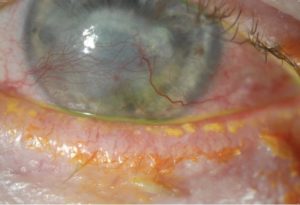
haritisBlepharitis is an inflammation of the eyelids. Like dry eye syndrome, it is often a chronic condition but can usually be controlled with treatment.
Blepharitis is often divided into anterior (involving the front aspect of the eyelids including the lashes) and posterior (involving the eyelid margin including the Meibomian glands). In reality, many eyes have both forms at the same time.
Blepharitis symptoms are very similar to dry eye symptoms. Blepharitis tends to cause more redness and crusting of the eyelids and the symptoms are often worse in the morning and improve throughout the day. Treatment depends partly on whether it is more anterior or posterior but generally includes a combination of warm compresses, eyelid scrubs, artificial tears, antibiotic drops or ointment, cyclosporine or lifitegrast and occasionally topical steroids or oral antibiotics. For eyelid inflammation not responding to medical therapy, an in-office Lipiflow procedure can often improve dryness symptoms by clearing out the Meibomian glands.
Ocular surface disease indicates damage to the surface layers of the eye, namely the cornea and conjunctiva. There are many causes ocular surface disease, but the 2 most common ones are “dry eye syndrome” and “blepharitis”.
The most common symptoms of dry eye syndrome are a dry, gritty, sandy sensation in the eyes, but symptoms also include redness, mucous discharge, fluctuation of vision, contact lens intolerance, and ironically, excess tearing. Many of these symptoms can also be caused by other ocular conditions such as blepharitis (inflammation of the eyelids) and ocular allergies. Dry eye symptoms are often made worse by activities where patients tend not to blink frequently, such as reading, working on the computer, and watching television. Dry eye symptoms are also generally worse toward the end of the day.
Blepharitis symptoms are very similar to dry eye symptoms. Blepharitis tends to cause more redness and crusting of the eyelids and the symptoms are often worse in the morning and improve throughout the day.
Dry eye syndrome is primarily caused by poor quality or quantity of tears.
Blepharitis means inflammation of the eyelids. Blepharitis is often divided into anterior (involving the front aspect of the eyelids including the lashes) and posterior (involving the eyelid margin including the Meibomian glands). In reality, many eyes have both forms at the same time.
Dry eye syndrome: advancing age, female, dry environment, smoking exposure, connective tissue disorder (e.g. Sjogren syndrome, rheumatoid arthritis), conjunctival scarring (e.g. from prior injury), certain medications (e.g. anti-histamines, beta-blockers), vitamin A deficiency, prior eye surgery, especially corneal refractive surgery.
Blepharitis: advancing age, rosacea, prior isotretinoin (e.g. Accutane) use
Corneal “dry spots”, corneal abrasions, corneal infections, corneal scarring, corneal thinning, corneal perforation.
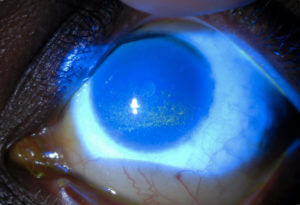
The diagnosis can usually be made during a slit lamp examination with special dyes such as fluorescein and lissamine green. Ancillary testing includes measurement of tear production (Schirmer’s test), and possibly measurement of tear saltiness (osmolarity) and tear inflammation (e.g. MMP-9). If Sjogren syndrome is suspected, a referral to a rheumatologist should be considered.
There is a stepwise approach treatment of dry eyes generally beginning with artificial teardrops, gels and ointments, cyclosporine drops (e.g. Restasis or Cequa), lifitegrast drops (e.g. Xiidra), and punctal plugs. Changing the local environment such as using humidifiers and staying away from drafts can also be very helpful. Other treatments include cautery of the tear drainage ducts (when plugs aren’t staying in), Lacriserts, acetylcysteine (Mucomyst) for mucous filaments, and permanent partial closure of the eyelids (small lateral tarsorrhaphy). Dry eye syndrome is often a chronic condition, but can usually be controlled with treatment.
Treatment depends partly on whether it is more anterior or posterior but generally includes a combination of warm compresses, eyelid scrubs, artificial tears, antibiotic drops or ointment, cyclosporine or lifitegrast and occasionally topical steroids or oral antibiotics. Blepharitis, like dry eye syndrome, is often a chronic condition, but can usually be controlled with treatment. For eyelid inflammation not responding to medical therapy, an in-office Lipiflow procedure can often improve dryness symptoms by clearing out the Meibomian glands.
Routine eye examinations are recommended to monitor the condition.
